Every once in a while, physicians face a patient with rather unspecific symptoms of exhaustion, sore muscles and joints, bad headache and sometimes even neurological deficits and paralysis. Only if the patient remembers or if the physician explicitly asks, may the cause be rapidly found: a tick bite – an indication that the person may be infected with Borrelia and is suffering from Lyme neuroborreliosis.
Important information about infection with Borrelia
- the bacterium Borrelia burgdorferi sensu lato causes Lyme borreliosis (Lyme disease) and is transmitted to humans by a tick bite
- Lyme neuroborreliosis is a severe form of Lyme disease in which the central and peripheral nervous systems are attacked by Borrelia
- Lyme neuroborreliosis is characterized by inflammation of (brain and spinal) meninges (meningoradiculoneuritis) and adjacent nerves and nerve roots resulting in pain, numbness and/or paralysis
Diagnosing a Borrelia infection
According to European guidelines, diagnosis of Lyme disease is based on the presence of characteristic symptoms and the detection of anti-Borrelia antibodies in patient’s serum. Additionally, an intrathecal antibody synthesis in cerebrospinal fluid (CSF) has to be demonstrated for diagnosis of acute Lyme neuroborreliosis. This is determined by calculation of the Borrelia–specific antibody index (serum/CSF). Serum and CSF samples have to be withdrawn on the same day and analyzed together.
Anti-borrelia antibody testing
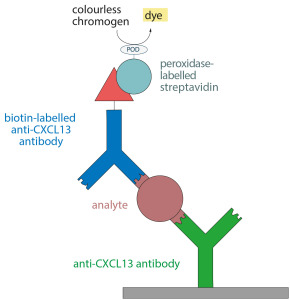
Usually, ELISAs are applied to screen serum or CSF of patients with suspected Lyme neuroborreliosis. The ELISA plates are coated with different antigens from Borrelia extracts which bind the corresponding anti-Borrelia antibodies in the sample. IgM antibodies against the Borrelia outer surface protein C (OspC) and IgG antibodies targeting the variable major protein-like sequence expressed (VlsE) belong to the first detectable anti-Borrelia antibodies in patients‘ sera.
What, however, if there is a negative test result with no detectable anti-Borrelia antibodies, although an infection with Borrelia is strongly suspected? An infection cannot be excluded with a negative result. In fact, specific anti-Borrelia antibodies cannot be detected in up to 20% of acute Lyme neuroborreliosis patients, especially in the early stages of infection. A new biomarker for acute Lyme neuroborreliosis may provide an answer to this diagnostic problem.
CXCL13 concentration increased in cases of acute Lyme neuroborreliosis
Over the past few years, scientists have researched the chemotactic cytokine (= chemokine) CXCL13 in the context with acute Lyme neuroborreliosis. Increased concentrations of the signalling molecule were found in the CSF of acute Lyme neuroborreliosis patients during different studies, even if the antibody index was not (yet) elevated.
CXCL13 is secreted by monocytes and dendritic cells, which have come into contact with the pathogens, and attracts B-cells into the CSF. After differentiation, the B-cells produce the specific anti-Borrelia antibodies. Therefore, an elevated CXCL13 level can be detected prior to the elevated antibody index. Additionally, the CXCL13 concentration is rapidly declining – in contrast to the antibody index – in patients under successful antibiotic therapy. Anti-Borrelia antibodies may persist especially in CSF for years despite a successful therapy, thereby hindering differentiation between acute and past Lyme neuroborreliosis.
Therefore, CXCL13 is a promising novel biomarker for improved Lyme neuroborreliosis diagnostics. Determination of the CXCL13 concentration using the new EUROIMMUN CXCL13-ELISA (order number: EQ 6811-9601-L) is suited to:
- supporting diagnosis of Lyme neuroborreliosis considering the characterstic symptoms – even in cases of a negative anti-Borrelia antibody finding,
- differentiating between acute and past Lyme neuroborreliosis,
- monitoring the course of therapy.
Still, it is important to mention that the CXCL13 concentration may be increased in other inflammatory infections of the central nervous system as well. These include e.g. lymphoma, viral infections or multiple sclerosis. Therefore, the complete clinical findings in CSF and symptoms have to be considered for diagnosis of Lyme neuroborreliosis.
